Cutting through the Regulatory Noise: Our new partnership with MedBoard
It seems that the medical device regulatory world has gone into overdrive in the last few years. The rate of regulatory change and the demand for clear guidance around them has substantially increased, especially when you focus on the European Union and the UK which are th key areas IVDeology specialise in. It is now getting to the point where one regultory expert simply cannot know everything they need to know, and this is without the peripheral requirements of REACH, CLP, Sustainability, Environmental and Digital. The need to find the right information from a trusted source has never been so important, as well as in a timely manner.
Our Regs Consultant Fiona Thompson commented the following:
“When I left my previous role to start at IVDeology, finding relevant, correct regulatory updates was one of the things I found most challenging. Having come from a large company, this was all done at a Corporate level and at our site we found out information from notifications or changes to the Global procedures sent out. Out of this corporate world, the places I knew where to look for information had all disappeared and trying to find all the potential websites to set up personnel alerts, I will be honest, was very painful – and I’m still sure I haven’t found them all.”
Even from the early days of IVDeology, the aim was to develop a strong team connected to a wide and diverse industry network, which would help us inform our customers on any Quality and Regulatory updates relating to IVDs and Medical Devices. We do this knowing that many of our SME customer don’t have this network themselves and getting the right information can be a very difficult and time-consuming thing.
Recently we have started using a system called MedBoard – and what a game-changer this is!
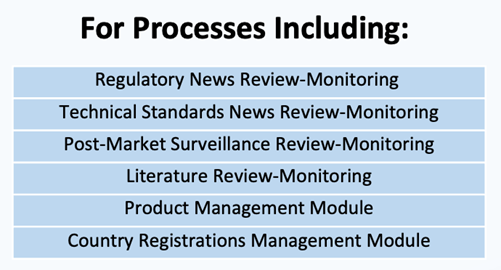
“MedBoard is a dedicated search engine for the sector. You can set up customised reviews with relevant key words to keep up to date with new regulatory news in specific countries that you are interested in as well as conduct searches for PMS, literature searches etc. It also sends you email alerts when new information is released. What MedBoard does is provide you with a starting point for regulatory intelligence, based on trusted resources, this allows you the opportunity to build your understanding and supplement your existing knowledge network.”
How do we use MedBoard to support our customers?
IVDeology have used the MedBoard subscription services since early 2023 as we personally find the subscription beneficial to cut through the noise and share the industry updates that are tailored and beneficial to our customers.
IVDeology is proud to funnel information down to our customers and recommend MedBoard’s services and be able to add:
a) timely regualatory updates from a trusted source
b) offer insights on the impact of these updates, using our in-depth knowledge of the IVD indsutry
The outcome for this is to give you the ability to make informed decisions, develop strategies and mitigate changes to the IVD industry relevant to your devices and markets.
At IVDeology, we don’t believe these is a one size fits all model for what we do, as we are committed to helping you in the way that works best.
We’re happy to be able to share updates from MedBoard and put you in touch if you wish to sign up individually as a company to be able to personalise the package at which level you wish, as MedBoard offer several layers of package support depending on budget and need including a new artificial intelligence scanning tool as well as software Validation documents approach for QMS/GxPs processes overviews.
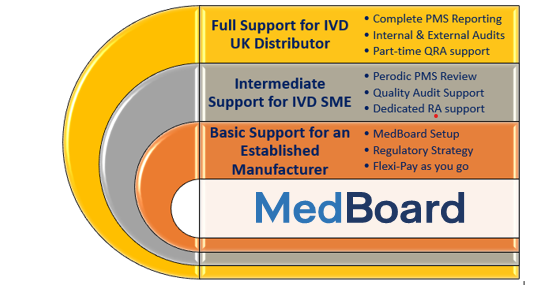
IVDeology adds a layer of support to help explain and discuss the updates and how this may affect your company, teams and projects. This sits well alongside our existing compliance services including UK Responsible Person (UKRP), Person Responsible for Regulatory compliance (PRRC), training, ad-hoc and project support. You can find more about these services on our website.
And to support one step further, IVDeology have a certified team of Quality experts in ISO9001 and ISO13485 to help with implementation of QMS systems and remediation, including software validation.
We don’t make anything from sign ups, we just really think the tool is an excellent creation, and side by side we can create a support system of clear updates whilst also breaking it down into easy digestible actions which saves you valuable time.
For further information or a demonstration on how we can help you, please book a call with Casey or drop us an email at [email protected] to know more.
