We are pleased to announce that on the 03rd May 2024, IVDeology Holdings Ltd (including IVDeology Limited and IVDeology UKRP Limited) have been acquired by Abingdon Health plc.
About Abingdon Health
Abingdon Health is a leading lateral flow contract research (CRO) and contract development and manufacturing organisation (CDMO) offering its services to an international customer base across industry sectors that include clinical, animal health, plant health, and environmental testing. Abingdon Health has the internal capabilities to take projects from initial concept through to routine and large-scale manufacturing; from “idea to commercial success.”
The Company’s CDMO division offers product development, regulatory support, technology transfer and manufacturing services for customers looking to develop new assays or transfer existing laboratory-based assays to a lateral flow format. Abingdon Health aims to support the increase in need for rapid results across many industries and locations and produces lateral flow tests in areas such as infectious disease, clinical testing including companion diagnostics, animal health and environmental testing. Faster access to results allows for rapid decision making, targeted intervention and can support better outcomes.
Abingdon Health’s Abingdon Simply Test™ range of self-tests is an ecommerce platform that offers a range of self-tests to empowers consumers to manage their own health and wellbeing. The Abingdon Simply Test™ ecommerce site offers consumers a range of information to support them in making informed decisions on the tests available. In addition, the site provides Abingdon’s contract services customers with a potential route to market for self-tests. The Abingdon Simply Test range is also sold through international distributors and through other channels in the UK and Ireland such as pharmacy chains.
Founded in 2008, Abingdon Health is headquartered in York, England.
For more information visit: www.abingdonhealth.com
Building on Quality and Regulatory Expertise
Nancy and Stuart created IVDeology in 2018 to provide support to IVD Manufacturers throughout their compliance journey, building long term relationships with our customers, suppliers and industry stakeholders. We have been honoured to support many projects throughout the EU IVDR and UKCA transitions, and helped deliver diagnostic tests and IVD accessories throughout the Covid-19 outbreak.
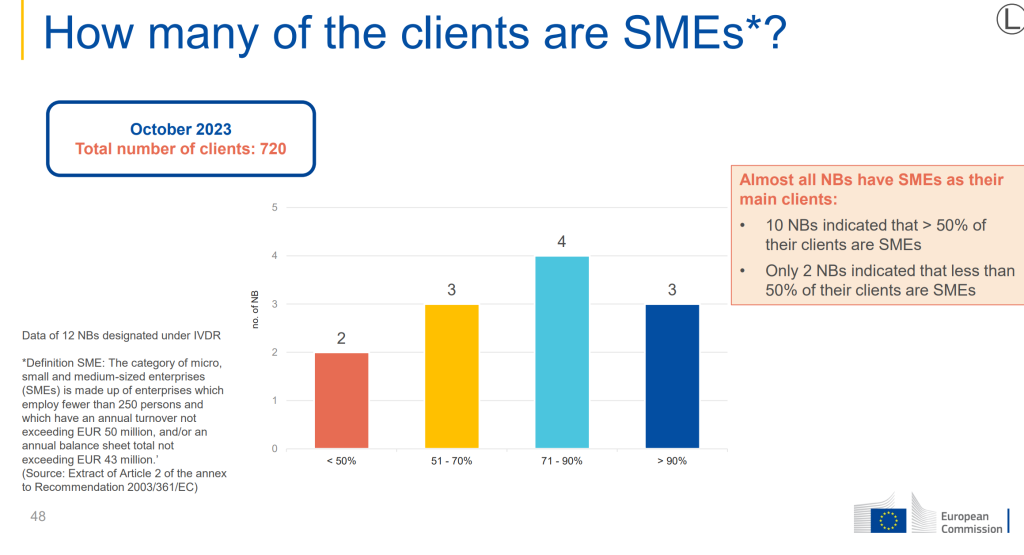
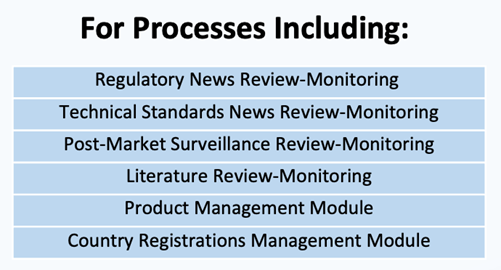
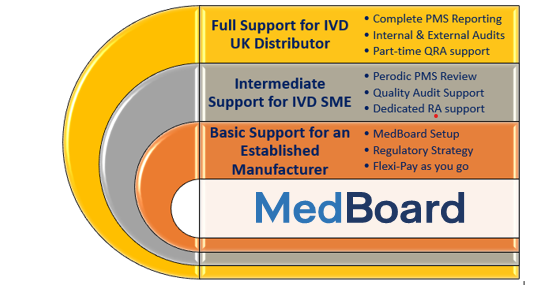
This opportunity builds on the continued growth and success of the IVDeology group providing expert regulatory, quality and compliance services to the in-vitro diagnostic industry. We have always welcomed collaboration with our strategic partners to be part of a holistic approach to deliver end to end support to the industry, from SME and micro businesses to large, multi-national IVD manufacturers. Stuart and Nancy will continue to lead IVDeology as part of the wider Abingdon Health group. We will also continue to work with our existing customers and partners, but be able to offer a wider range of connected services via Abingdon Health in conjunction with the existing Quality and Regulatory services.
Stuart Angell, Managing Director IVDeology commented:
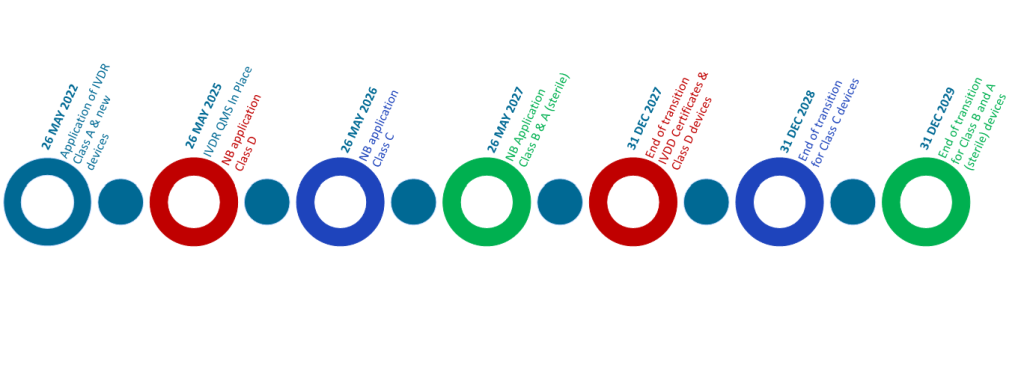
Myself, Nancy and the rest of the IVDeology team are excited to be joining the Abingdon Health Group. The in vitro diagnostics sector is under a significant period of regulatory change in the UK, EU and internationally. By combining our collective skills, knowledge and expertise, we can support our customers and the wider IVD industry with the collective breadth of knowledge that this opportunity provides.
Chris Yates, CEO, commented:
“We’re delighted to welcome Stuart, Nancy and the rest of the IVDeology team to the Abingdon Health group. The acquisition of IVDeology is in line with Abingdon’s strategy of providing our customers with all the pieces of the jigsaw required to bring products from idea to commercial success. The IVDeology team will strengthen Abingdon’s existing knowledge leadership and regulatory expertise. We look forward to working with the IVDeology team and supporting existing and new customers in navigating a regulatory environment going through a period of significant change.”
Signed Stuart Angell, MD of IVDeology Ltd